Long waits in emergency departments are a symptom of an unsustainable health system, one that relies too heavily on hospital care and doesn’t do a good job coordinating care options in the community. Considerable time and effort have been invested – in Saskatchewan and elsewhere – to identify solutions to this complex, long-standing problem.
Saskatchewan’s new Connected Care strategy is about providing the right care, at the right time, in the right place, with the right provider. The Emergency Department Waits and Patient Flow Initiative housed at HQC explored different strategies our province could use to shorten waits in Emergency and improve the patient journey throughout the health care system.
HQC staff who were part of the Initiative have summarized the Top 10 “simple” concepts from our learnings that we can use in Saskatchewan to tackle this problem. Although the concepts themselves are relatively straightforward, implementing them is not. The good news is that there are teams across the province who are already applying these approaches; we can learn and draw inspiration from them. In this post we summarize the top 10 Connected Care lessons learned and provide examples of how local teams are implementing these strategies.
Our Top 10 lessons learned in Connected Care (with local examples)
Lesson 1: Build care teams

In health care, we need teams of people who work toward a shared goal and trust each other. We know that high-functioning teams work well together, manage conflict, have a shared purpose, and lead collaboratively. Psychological safety is a key attribute of effective teams in any industry.
Build care teams: Saskatchewan example
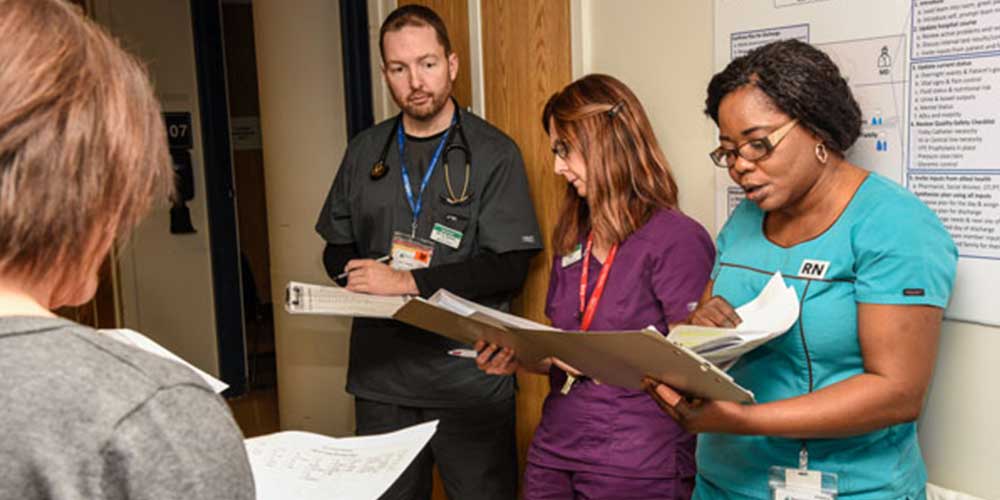
Teams working at Pasqua Hospital in Regina are using structured interdisciplinary bedside rounds (SIBR) to work together to deliver patient-centred care. If you want to learn more about this work, contact Dr. Kish Lyster via email or on Slack.
Build care teams: Recommended resources
- Health care professional development: Working as a team to improve patient care
- BC Patient Safety and Quality Council’s resource on Activities for Transforming Teams & Igniting Change
Lesson 2: Create intermediate care teams

Saskatchewan has an aging population with increasingly complex care needs. We need a new type of care team that bridges the gap between hospital care and typical primary care and home care services.
Intermediate care teams: Saskatchewan example
A team is working in Saskatoon’s Market Mall area to provide specialty services for people over age 50. The team’s services bridge the gap between hospital and primary care services. If you want to learn more about the work the team is doing, contact Don Brophy via email or on Slack.
Intermediate care teams: Recommended resource
- The health system in Canterbury, New Zealand has redesigned services to meet the needs of their population.
Lesson 3: Get patients moving

Getting hospital patients up and out of bed regularly and into their own clothes can help them go home sooner and stronger. Older patients, in particular, lose muscle strength when they’re inactive, putting them at risk for a longer hospital stay or being moved to long-term care instead of going home.
Get patients moving: Saskatchewan example
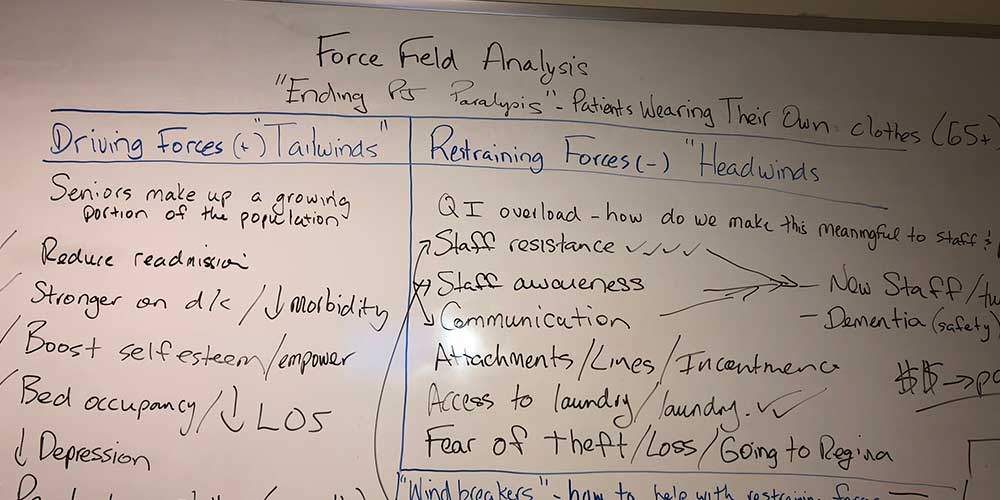
Curtis Newton, a physiotherapist in Swift Current, is working with his colleagues in that community to organize a #endPJparalysis campaign, to get patients over 65 up and about, and dressed in their own clothes. On the whiteboard pictured above, the team has listed the different factors that will help and hinder their campaign. If you want to learn more about this work, connect with Curtis via email or on Slack.
Get patients moving: Recommended resource
Lesson 4: Prioritize continuity

There are three types of continuity that are essential to well-coordinated health care: 1) continuity in relationships; 2) continuity in management; and, 3) continuity in information. The High-Quality Care Transitions bridge below illustrates the different processes that support continuity.
Prioritize continuity: Saskatchewan example
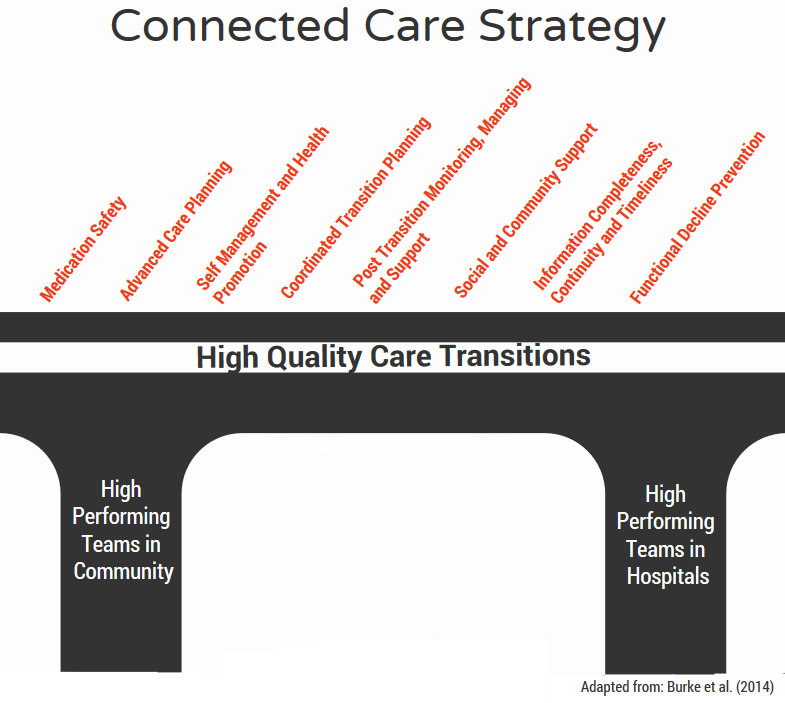
Two teams in Saskatoon are partnering to implement the elements of high-quality care transitions for patients who receive care at St. Paul’s Hospital and in the Market Mall area. If you want to learn more about the work the team is doing, contact Pam Molnar via email at or Graham Fast.
3sHealth has improved information flow and clinical management through the introduction of self-edit voice recognition technology; now it’s easier and faster for physicians to capture information from patient visits. For more information about this, email Joy Dobson.
Prioritize continuity: Recommended resource
- High-Quality Care Transitions: A Guide to Improving Continuity of Care (Online Guide)
- Video: Clinical intelligence feature of self-edit voice recognition software
Lesson 5: Optimize ED processes

In Saskatchewan, there is work underway to improve processes within Emergency. We are using health system modelling to determine what impact reducing delays in access to lab, imaging, and consultations will have on wait times. While we wait for those results, we can apply recommendations from Choosing Wisely to reduce unnecessary tests within the emergency department.
Optimize ED processes: Recommended resources
Lesson 6: Involve physicians as partners

Every high-performing health care system in the world actively involves physicians in designing and implementing improvements. In Saskatchewan, physicians and other clinicians are learning how to become leaders in clinical quality improvement initiatives through the Clinical Quality Improvement Program (CQIP).
Involve physicians as partners: Saskatchewan example

At St. Joseph’s Hospital in Gravelbourg, Dr. Intheran Pillay co-leads their interdisciplinary bedside rounding, alongside nurse manager Desiree Brisebois. If you want to learn more about the work the team is doing, contact Desiree via email or on Slack.
Involve physicians as partners: Recommended resource
- The Evolving Professional Relationship Between Canadian Physicians and the Health Care System: Where do we stand (Canadian Medical Association)
Lesson 7: Integrate our approach
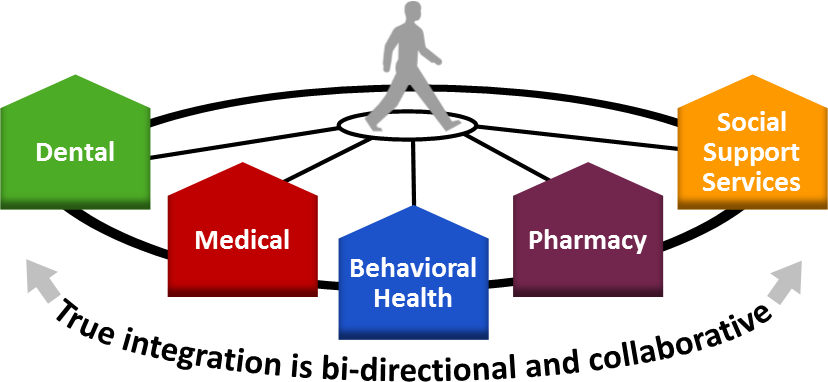
Acute and community care teams can develop a deeper understanding of the physical, mental, cultural, and social care needs of the people they serve, which can help prevent hospital admissions, readmissions, and premature placement in long-term care.
Integrate our approach: Saskatchewan example

The Hub in Prince Albert (Community Mobilization Prince Albert) is a great example of how agencies working in different sectors can combine their expertise to address complex human and social problems. For more information about HUB tables in Saskatchewan, check out the recording of our June 2018 QI Power Hour session, or contact Matt Gray or Sarah Collins.
Integrate our approach: Recommended resource
- Improving Community Health and well-being in Saskatchewan (QI Power Hour)
Lesson 8: Align measurement systems

In health care, providers check a patient’s vital signs – heart rate, pulse, temperature – to assess their current condition. In the same way, we need a set of key measures we can use to determine the status of the health system. One of these system vital signs is the percentage of unnecessary days in hospital, also known as alternate level of care (or ALC).
Align measurement systems: Saskatchewan example
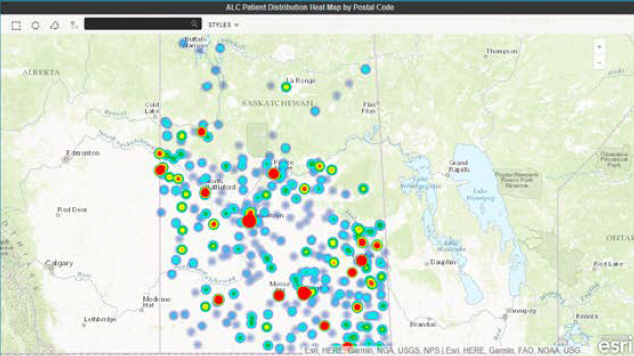
The Alternate Level of Care Dashboard created by eHealth Saskatchewan shows the home community of those people in hospital who no longer require acute care. This information is critical to determine what community-based services are needed and where.
Align measurement systems: Recommended resource
- An example of a system-level measurement framework in New Zealand
Lesson 9: Start a big conversation

We need to shift the conversation away from talking about the need for more hospital and long-term care beds, to focus on how to better meet people’s care needs closer to home in the community.
Start a big conversation: Recommended resource
- Examples of campaigns that are shifting the conversation are #endPJparalysis and #last1000days.
Lesson 10: Ask: “What matters to you?”
In 2009 Saskatchewan conducted an extensive consultation – the Patient First Review – to hear from citizens what matters most to them when it comes to their health care. In our daily interactions with patients, we can ask that same question: What matters to you?
What matters to you? Saskatchewan example
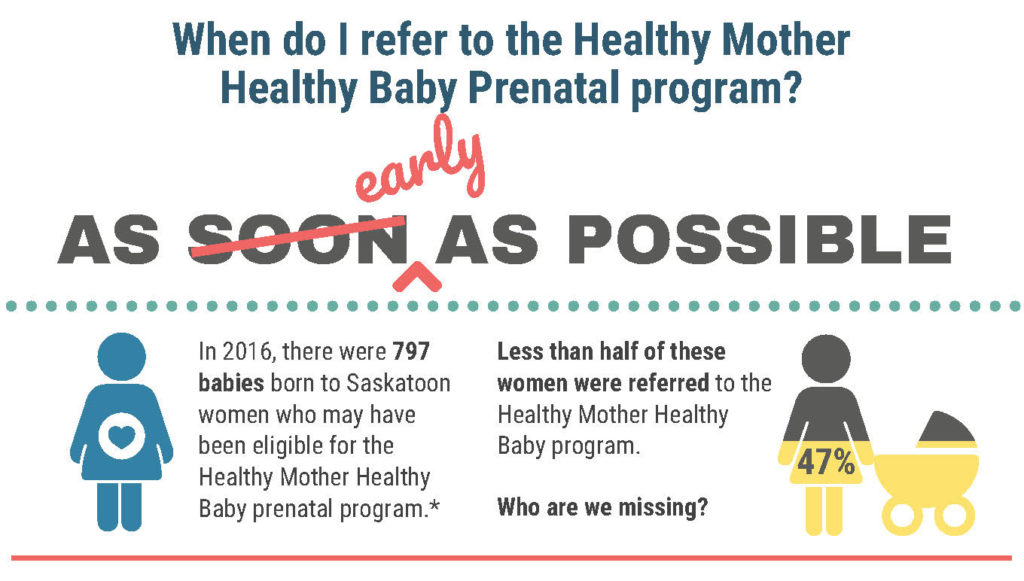
The team at Healthy Mother Healthy Baby in Saskatoon is asking their clients what matters to them. Through this work, they found that many mothers don’t have a birth certificate card, which makes it more difficult for them to access income security and housing. In response, the Healthy Mother Healthy Baby team is conducting an improvement project to make it easier for mothers to get birth certificates. If you want to learn more about the work the team is doing, contact Jacki Veregin via email.
What matters to you? Recommended resource
Connected Care: How you can get involved
Do you want to get started with connected care? You can:
- share your ideas with your managers and directors, and let them know what you can do to help;
- print off the new Lessons Learned infographic; it’s a great tool to help you start a discussion; or,
- inspire your staff to test improvement ideas related to the different lessons.
We can all contribute to creating connected care in Saskatchewan!




